Sleep Medicine
What is Sleep Apnea?
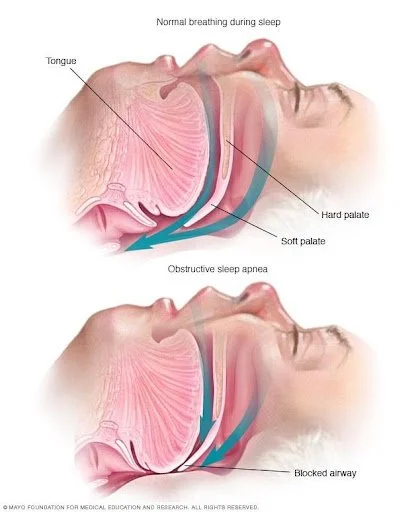
Sleep Apnea is the failure to breathe while you sleep. Obstructive Sleep Apnea is the most common type of sleep apnea. In this form of the disease, the airway collapses, cutting off air flow to the lungs. Snoring is often associated with poor sleep; sometimes overlooked by the patient, although not by their bed partner! A partial airway obstruction causes the upper airway tissues to vibrate and produce the sound of the classic snore. The second and uncommon type of sleep apnea is the Central Sleep Apnea, where there is reduced drive by the brain to take breaths when the person sleeps.
Risk factors
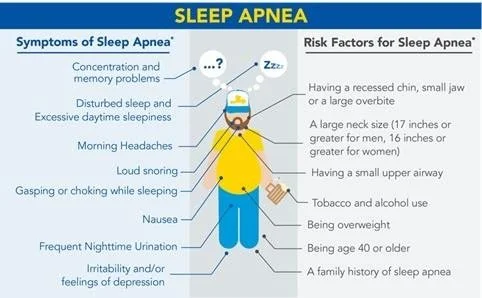
Sleep apnea can affect anyone, even children. But certain factors increase your risk as listed below.
Excess weight. Obesity greatly increases the risk of sleep apnea. Fat deposits around your upper airway can obstruct your breathing.
Neck circumference. People with thicker necks might have narrower airways.
A narrowed airway. You might have inherited a narrow throat. Tonsils or adenoids also can enlarge and block the airway, particularly in children.
Being male. Men are two to three times more likely to have sleep apnea than are women. However, women increase their risk if they're overweight, and their risk also appears to rise after menopause.
Being older. Sleep apnea occurs significantly more often in older adults.
Family history. Having family members with sleep apnea might increase your risk.
Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat, which can worsen obstructive sleep apnea.
Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who've never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway.
Nasal congestion. If you have difficulty breathing through your nose — whether from an anatomical problem or allergies — you're more likely to develop obstructive sleep apnea.
Symptoms
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making it difficult to determine which type you have. The most common signs and symptoms of obstructive and central sleep apneas include:
Loud snoring
Episodes in which you stop breathing during sleep — which would be reported by another person
Gasping for air during sleep
Awakening with a dry mouth
Morning headache
Difficulty staying asleep (insomnia)
Excessive daytime sleepiness (hypersomnia)
Difficulty paying attention while awake
Irritability
Is it Just Snoring or is it Sleep Apnea?
Not everyone who snores has sleep apnea, and not everyone who has sleep apnea snores. So how do you tell the difference between garden variety snoring and a more serious case of sleep apnea?
The biggest telltale sign is how you feel during the day. Normal snoring doesn't interfere with the quality of your sleep as much as sleep apnea does, so you're less likely to suffer from extreme fatigue and sleepiness during the day.
Diagnosis of Sleep Apnea
As with other medical conditions, the process of diagnosing the condition and assessing the severity of it starts with initial suspicion. The patient, or their partner might bring out symptoms. The physician might suspect it based on your complaints or other associated medical condition, or your body habitus, neck and oropharyngeal configuration.
Sleep Screening Questionnaires are available that can be a good initial start, and document the need for a sleep test. The sleep test can be done in a lab or in the comfort of your own bed at home.
Testing in a Sleep Lab
This will require you to go to a sleep center and spend the night in their facility. In order to evaluate you for a number of sleep diseases, electrodes will be attached to your head and body to perform a full sleep study. In some labs, you may try on a Continuous Positive Airway Pressure (CPAP) mask and see what therapy is like should you need it.
Home Sleep Testing
You may be prescribed a home sleep test. This offers an easier option, as you will be able to spend the night in your own bed in familiar surroundings. After a brief training by your healthcare provider, you can take home a home sleep testing device for a self-administered sleep test. This could save you and/or your insurance company money, as the typical cost of a home sleep test is only a fraction of the cost of an in-lab sleep test. It can be especially advantageous to the home-bound, elderly, or those with chronic illnesses, who require specialized care such as a nurse or a trained family member. It can avoid expensive transportation costs. It is also beneficial for those with trouble arranging time out of their schedules to spend the night in a sleep lab.
Why Sleep Apnea is harmful - The Cumulative Effect of Sleep Apnea
As Obstructive Sleep Apnea (OSA) develops, it has a cumulative effect. This means that the longer the disease goes untreated, the greater the negative effects and associated health risks. If sleep apnea remains untreated, other health conditions may emerge or current health problems may heighten, including:
High Blood Pressure: especially important to diagnose in a younger person with high blood pressure
Heart Diseases: including heart attacks, heart failure, arrhythmias, atrial fibrillation, pulmonary hypertension.
Heart Attack
Heart Failure
Stroke
Diabetes
Depression
Reflux disease (GERD)
Atherosclerosis
Gestational Diabetes
Sexual Dysfunction
Excessive daytime sleepiness
Difficulty concentrating on tasks such as driving and remaining focused at meetings. (Fatal car accidents are increased seven fold)
Morning and daytime headaches
Generalized irritability
Impaired emotional functioning
Sleep disordered breathing in childhood may be instrumental in delaying or damaging cognitive development.
Treatment
Various treatments can be grouped under the following headings, and in general serve an increasing severity of the obstructive sleep apnea.
Lifestyle changes and weight loss:
CPAP/BiPAP
Oral appliances
Surgical therapy and Pacemaker
Lifestyle and Weight loss
These care tips might suffice in the very mild cases, but always should be followed in addition to more definitive therapy as outlined below.
Lose excess weight. Even a slight weight loss might help relieve constriction of your throat. In some cases, sleep apnea can resolve if you return to a healthy weight, but it can recur if you regain the weight.
Exercise. Regular exercise can help ease the symptoms of obstructive sleep apnea even without weight loss. Try to get 30 minutes of moderate activity, such as a brisk walk, most days of the week.
Avoid alcohol and certain medications such as tranquilizers and sleeping pills. These relax the muscles in the back of your throat, interfering with breathing.
Sleep on your side or abdomen rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway. To keep from rolling onto your back while you sleep, try attaching a tennis ball to the back of your pajama top. There are also commercial devices that vibrate when you roll onto your back in sleep.
Don't smoke. If you're a smoker, look for resources to help you quit.
Breathe right nasal strips, and keeping the nasal passages open. Saline spray, anti-allergy medications and breathing exercises can help.
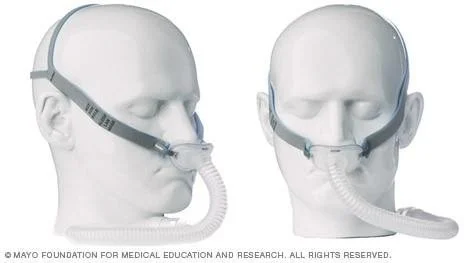
Continuous Positive Airway Pressure and Bi-Level Positive Airway Pressure (CPAP and BiPAP)
CPAP is the most common treatment for obstructive sleep apnea. CPAP is non-invasive (it does not enter the body). The CPAP machine is small and pulls in room air, and blows it into a tube which is attached to a mask worn by the patient. The pressurized air from the CPAP keeps the airway open, allowing the patient to breathe.
Although CPAP is the most common and reliable method of treating sleep apnea, some people find it cumbersome or uncomfortable. Some people give up on the CPAP machine, but with practice, most people learn to adjust the tension of the straps on the mask to obtain a comfortable and secure fit. Living with this machine is a learning process.
You might need to try more than one type of mask to find one that is comfortable. Don't stop using the CPAP machine if you have problems. Check with your doctor to see what changes can be made to increase your comfort.
Additionally, contact your doctor if you're still snoring or begin snoring again despite treatment. If your weight changes, the pressure settings of the CPAP machine might need to be adjusted.
Some CPAP machines can automatically adjusts the pressure while you're sleeping (auto-CPAP). Units that supply bilevel positive airway pressure (BiPAP) also are available. These provide more pressure when you inhale and less when you exhale ,and improve the tolerability of this treatment modality.
Oral appliances
Another treatment option is wearing an oral appliance designed to keep your throat open. CPAP is more reliably effective than oral appliances, but oral appliances might be easier to use. Some are designed to open your throat by bringing your jaw forward, which can sometimes relieve snoring and mild obstructive sleep apnea. Some of these devices hold your tongue down and forward.
A number of devices are available even without prescription off the internet, but some dentists specialize in making custom devices with your oral measurements
Once you find the right fit, you'll need to follow up with your dentist repeatedly during the first year and then regularly after that to ensure that the fit is still good and to reassess your signs and symptoms.
Surgical therapy and Pacemaker
Surgery is usually only an option after other treatments have failed. Generally, at least a three-month trial of other treatment options is suggested before considering surgery. However, for a small number of people with certain jaw structure problems, it is a good initial option.
Surgical options might include:
Tissue removal. During this procedure (uvulopalatopharyngoplasty), your doctor removes tissue from the rear of your mouth and top of your throat. Your tonsils and adenoids usually are removed as well. This type of surgery might be successful in stopping throat structures from vibrating and causing snoring. It is less effective than CPAP therapy.
Radiofrequeny ablation: Removing tissues in the back of your throat with radiofrequency energy might be an option if you can't tolerate CPAP or oral appliances. In this treatment, tissue at the rear of your mouth and the back of your throat is shrunk using radiofrequency ablation. This procedure might be used for mild to moderate sleep apnea.
Jaw repositioning. In this procedure, your jaw is moved forward from the remainder of your face bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely. This procedure is known as maxillomandibular advancement.
Implants. Plastic rods are surgically implanted into the soft palate after you've received local anesthetic. More research is needed to determine how well implants work.
Inspire Pacemaker Nerve stimulation. This requires surgery to insert a stimulator for the nerve that controls tongue movement (hypoglossal nerve). The increased stimulation helps keep the tongue in a position that keeps the airway open.
Creating a new air passageway (tracheostomy). You may need this form of surgery if other treatments have failed and you have severe, life-threatening sleep apnea. In this procedure, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. You keep the opening covered during the day. But at night you uncover it to allow air to pass in and out of your lungs, bypassing the blocked air passage in your throat.
Weight-loss (bariatric) surgery